Mental Health Conditions › OCD
+ What is it | + Symptoms | + Causes | + Treatment | + Videos
OCD is a chronic mental health condition that is usually associated with obsessive thoughts and compulsive behaviour.
Obsessions and compulsions
An obsession is an unwanted, unpleasant thought, image or urge that repeatedly enters a person’s mind and results in anxiety. A compulsion is a repetitive behaviour or mental act that a person feels compelled to perform to try to avert or undo the effect of the obsession.
Unlike the normal use of the word ‘obsession’, which may describe something that an individual enjoys, the obsession in OCD is unpleasant and frightening. The person feels the need to carry out their compulsion in order to prevent their obsession becoming true. For example, someone who is obsessively scared that they will catch a disease may feel compelled to have a shower every time they use a toilet.
How common is OCD?
OCD is one of the most common mental health conditions. It is estimated that up to 3 in 100 adults and up to 5 in 100 children and teenagers have OCD.
OCD usually starts in early adult life, with men tending to report earlier symptoms than women. However, OCD symptoms can begin at any time, including childhood.
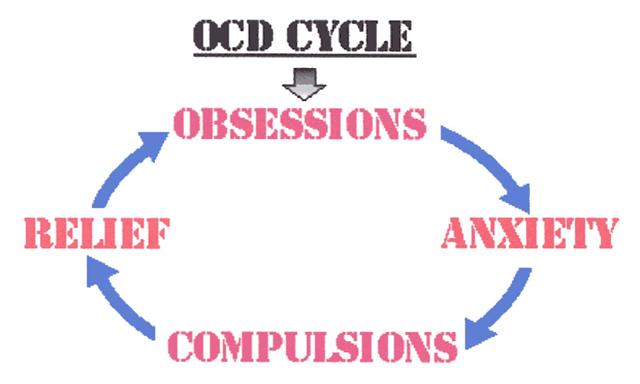
While OCD is a condition that can affect people differently, it usually causes a particular pattern of thought and behaviour. The 4 main steps of this pattern are:
- Obsession: Mind is overwhelmed by a constant obsessive fear or concern
- Anxiety: Obsession provokes feelings of intense anxiety
- Compulsion: Adopt a compulsive pattern to reduce anxiety
- Relief: Compulsion brings relief from anxiety for a short time. Obsession & anxiety return. Pattern repeats
While the exact causes of OCD are not known, a number of factors are thought to be involved in the development of OCD. These are: Genetic factors, brain abnormalities, serotonin, infection, life events, family involvement
Genetic Factors
Evidence suggest that OCD may be inherited in certain genes that affect the development of the brain. Evidence also suggests that OCD runs in families. A person with OCD is 400% more likely to have another family member with OCD
OCD is also thought to be linked to other conditions such as tics and Tourette's syndrome
Brain Abnormalities
Studies of brain images have shown that people with OCD have abnormalities in some parts of the brain - such as increased blood flow and increased brain activity
The affected areas of the brain are the areas that deal with strong emotions and the responses to these emotions. The studies also showed that successful treatment with CBT or SSRIs showed a return to normal brain activity
Serotonin
Serotonin seems to play a part in OCD. Serotonin is a neurotransmitter
It is unclear how serotonin contributes to OCD, but medication that increases serotonin levels have successfully helped to treat the symptoms of OCD
Infection
Reports have shown that some children and young people develop OCD after an infection caused by streptococcal bacteria. It is quite possible that the antibodies produced by the body react with the brain and cause OCD
Life Events
Any adverse life event such as a bereavement or a family break-up is thought to trigger OCD in people with a tendency to the condition - such as those with genetic factors
This life event could also affect the course of the condition. The death of a loved one could trigger a fear that someone in the family may be harmed. Stress is thought to make OCD a lot worse, but is not a cause of the condition
Family Involvement
Upbringing is not thought to cause OCD. There are some factors, however, that could make OCD more likely to develop.
It is very unhelpful to a person suffering with OCD to involve family. Family will want to constantly reassure the person to make them feel better and this will prevent them seeking neccessary treatment
For people with OCD, treatment will involve the following:
- Treatment plan
- Behavioural therapy
- Medicines
Treatment Plan
OCD that causes mild functional impairment will involve a short course of CBT
OCD that causes moderate functional impairment will involve a more intensive course of CBT or taking SSRIs
OCD that causes severe functional impairment will require referral to a CMHT for a combination of intensive CBT and a course of SSRIs
Behavioural Therapy
Behavioural therapy will involve CBT and Exposure and response prevention.
ERP involves identifiying a number of situations that cause you anxiety. These are placed in order from causing the most anxiety to the least anxiety.
You and your therapist will identify certain tasks that expose you to the situation that causes you the anxiety, but at a level that you can cope with. You will need to do the ERP tasks but without carrying out the compulsions that help you cope with the situation.
This may sound like a frightening task for you. People with OCD who tackle and confront the anxiety without the compulsion, tend to find that the anxiety disappears in 1 - 2 hours.
This same exposure task should be carried out 2 - 3 times a day. As you do it, the anxiety is more likely to decrease and last for a shorter period of time. Once you have conquered this step, you can move on to a more difficult task until you have overcome all the situations that make you anxious.
For those with mild to moderate OCD, a 10 hour course of therapist treatment and self-treatment exposure exercises is all that is needed. For moderate to severe cases, a course of more than 10 hours is generally needed.
Medicines
The medicines used to treat OCD are SSRIs (such as Escitalopram) and TCAs (such as Clomipramine)